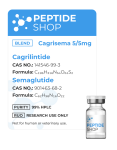
Cagrisema 10mg
Size: 10mg
Contents: 5mg Cagrilintide / 5mg Semaglutide
Form: Lyophilized powder
Purity: >99%
$165.00
| Quantity: | 10mg |
|---|---|
| Unit: | 1 vial |
| Contents: | Cagrisema |
| Form/Appearance: | Lyophilized/Powder |
| Peptide Purity: | 99% |
| Sequence: | Not Available |
| Molecular Mass: | Not Available |
| Solubility: | Sterile / Bacteriostatic water |
| Synonyms: | Cagrilintide/Semaglutide |
FAQs
Related Products
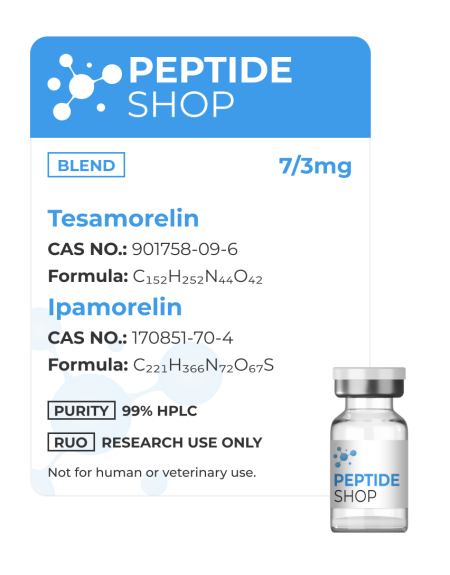
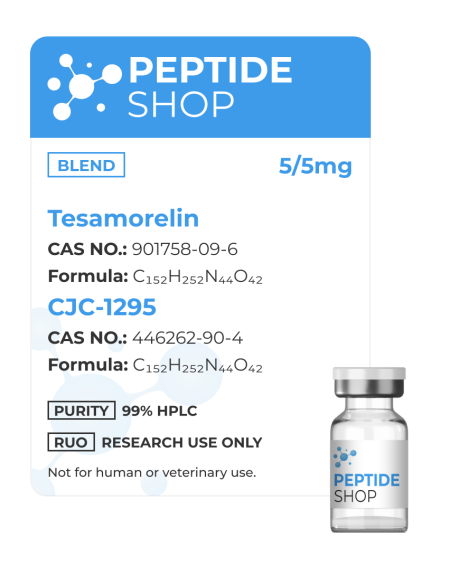
Tesamorelin and Ipamorelin are two peptides combined in a blend that seems to be sharing the potential to stimulate the growth hormone axis, although through different mechanisms. This combination might activate the pituitary gland, which further results in the release of endogenous growth hormone. The blend seems to be showing positive effects on mammals and primates in terms of sleep, lipid profile, mean mass, muscle tissues, cognition, and metabolic function.
Chemical Structure
Molecular Formula
- Tesamorelin: C152H252N44O42
- Ipamorelin: C221H366N72O67S
Molecular Weight
- Tesamorelin: 5136 g/mol
- Ipamorelin: 711.9 g/mol
Sequence
- Tesamorelin: Unk-Tyr-Ala-Asp-Ala-Ile-Phe-Thr-Asn-Ser-Tyr-Arg-Lys-Val-Leu-Gly-Gln-Leu-Ser-Ala-Arg-Lys-Leu-Leu-Gln-Asp-Ile-Met-Ser-Arg-Gln-Gln-Gly-Glu-Ser-Asn-Gln-Glu-Arg-Gly-Ala-Arg-Ala-Arg-Leu-NH2
- Ipamorelin: H-Aib-His-D-2Nal-D-Phe-Lys-NH2
Tesamorelin and Ipamorelin Blend – GH Deficiency
Tesamorelin is an analog of the growth hormone-releasing hormone. It binds GHRG receptors on somatotrophs in the pituitary gland. Considering that it promotes the release of GH, Tesamorelin could boost lipolysis, reduce visceral adipose tissue, and potentially improve glucose metabolism.
Ipamorelin is a GHSR antagonist as well. However, it appears to be activating GHSR in the peripheral tissues and hypothalamus, potentially causing the release of GH. Researchers suggest that since GHSR stimulates the increase of GH secretion, it can promote lipolysis, protein synthesis, and IGF-1 production.
When combined, these two compounds target different components of the GH axis. This dual action seems to positively affect and amplify the overall GH, like insulin sensitivity, lipid profile, body composition, and overall metabolic function in a laboratory setting.
Tesamorelin and Ipamorelin Blend and Type 2 Diabetes
Research has shown that both Tesamorelin and Ipamorelin may help manage blood sugar levels and address metabolic issues in people with Type 2 Diabetes (T2DM). Tesamorelin works by boosting the body’s own production of growth hormone, which experts believe improves how the body responds to insulin and uses glucose. On the other hand, studies on Ipamorelin suggest it may positively affect insulin sensitivity and glucose regulation. When used together, these peptides could offer combined benefits, potentially leading to lower HbA1c levels, better insulin sensitivity, and reduced abdominal fat with T2DM.
Other benefits
- In animal models, this blend seems to have a positive effect on the following:
- Cognitive improvement – may improve memory and learning abilities.
- Muscle density – might enhance muscle density and size.
- Appetite and digestion – according to one research, animals that were given this blend managed to decrease their weight by 15%.
References:
Adrian S, Scherzinger A, Sanyal A, Lake JE, Falutz J, Dubé MP, Stanley T, Grinspoon S, Mamputu JC, Marsolais C, Brown TT, Erlandson KM. The Growth Hormone Releasing Hormone Analogue, Tesamorelin, Decreases Muscle Fat and Increases Muscle Area in Adults with HIV. J Frailty Aging. 2019;8(3):154-159. doi: 10.14283/jfa.2018.45. PMID: 31237318; PMCID: PMC6766405.
Clemmons DR, Miller S, Mamputu JC. Safety and metabolic effects of tesamorelin, a growth hormone-releasing factor analogue, in patients with type 2 diabetes: A randomized, placebo-controlled trial. PLoS One. 2017 Jun 15;12(6):e0179538. doi: 10.1371/journal.pone.0179538. PMID: 28617838; PMCID: PMC5472315.
https://pubchem.ncbi.nlm.nih.gov/compound/Tesamorelin#section=Deprecated-CAS
Stanley TL, Chen CY, Branch KL, Makimura H, Grinspoon SK. Effects of a growth hormone-releasing hormone analog on endogenous GH pulsatility and insulin sensitivity in healthy men. J Clin Endocrinol Metab. 2011 Jan;96(1):150-8. doi: 10.1210/jc.2010-1587. Epub 2010 Oct 13. PMID: 20943777; PMCID: PMC3038486.
https://www.sciencedirect.com/science/article/abs/pii/S1096637401902394?via%3Dihub
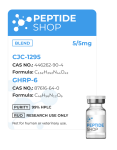
Size: 10mg
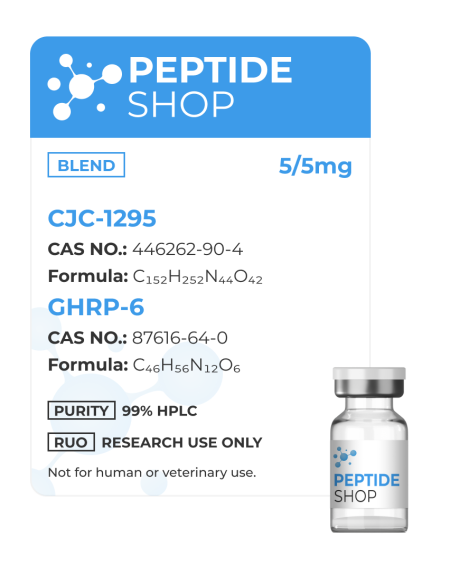
Contents: 5mg CJC-1295/ 5mg GHRP-6
Form: Lyophilized powder
Purity: >99%
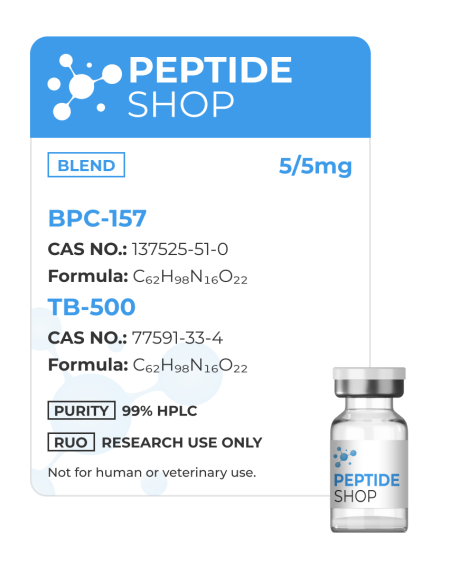
Though we sell BPC-157 and TB-500 individually, we’re also offering this peptide blend to our customers. Both BPC-157 and TB-500 are body protecting compounds naturally occurring in the GI tract, and animal research showed that, when using them in combination, they help repair the GI tract, increase the rate of repair and development of new blood vessels and generally speed up tissue recovery and healing.
Though these peptides act effectively when applied individually, due to the nature of their mechanism of action, they do not compete against each other, but work in conjunction to offer far more superior effects. Of course, these effects have yet to be tested in human test subjects, but animal testing demonstrated high effectiveness in healing and repair.
BPC-157, TB-500 Blend Effects
As previously mentioned, this peptide blend is especially effective in healing and recovery, in animal studies. Here is what the researchers found:
- It helps with injury protection
- Boosts joint flexibility
- Speeds up regenerative processes within the body
- Increases the rate of new blood vessels forming
- Improves gut health and heals intestinal walls
- It may improve physical endurance
- Enhance brain health
- Boost muscle growth and repair damaged bones and joints
Though, individually, both BPC 157 and TB 500 express these effects, this blend supercharges them, allowing for far more powerful end results.
Sadly, we still don’t have many studies showing the effect of this blend in humans, this is why this peptide blend is only available for laboratory research and scientific experiments. But as these experiments continue to progress, we will soon have more information from human test subjects.
Wound and Injury Repair Studies
Studies involving BPC-157 and TB-500, both in combination and individually, clearly showed that these peptides stimulate wound healing and recovery and injury repair. Of course, the majority of these studies were done on animals, and this is where we’re getting our data.
These studies further showed this peptide blend being effective in complete recovery from bone, muscle, joints and connective tissues injuries. Furthermore, BPC-157 and TB-500 blend showed a substantial prophylactic effect, encouraging stronger, more elastic and more durable musculoskeletal structures.
Growth Hormone Effects
This blend’s muscle building and wound healing recovery effect is tied closely to its ability to interact with growth hormone, as shown in animal studies. BPC and TB have a synergistic effect in which BPC 157 accelerates the expression of GH receptors on fibroblasts, which increases the longevity of these cells; while TB 500 increases the rate of wound healing when these GH receptors get activated.
This synergistic effect is what scientists are counting on, to develop a potent wound healing treatment designed to be faster and more effective to those being employed currently. This is why we are eager to see what future development and human studies will show.
BPC-157 and TB-500 Blend Side Effects
When talking about human use, this is the most important question scientists are looking to answer – is this blend safe for human use and does it come with any side effects?
Fortunately for us, individually, these peptides showed safe for use and not dangerous at all; same goes for the blend. But we need to keep in mind that this information comes from animal studies, so until we get some definitive human test subject studies, we won’t know for sure.
Until that happens, PeptideShop.com is only selling BPC-157/TB-500 blend for laboratory research!
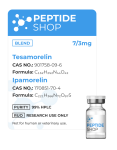
Size: 10mg
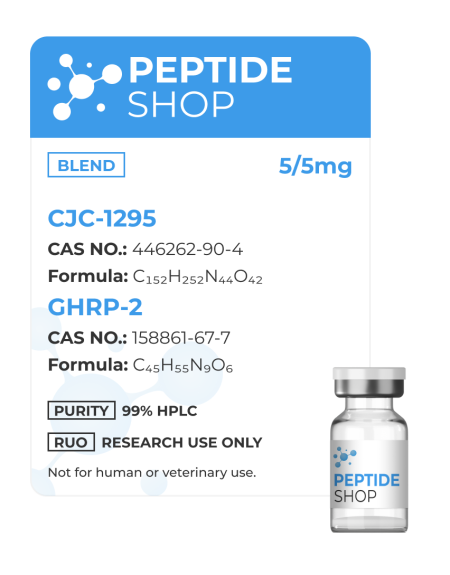
Contents: 5mg CJC-1295/ 5mg GHRP-6
Form: Lyophilized powder
Purity: >99%
Size: 10mg
Contents: Sermorelin 5mg, Ipamorelin 5mg
Form: Lyophilized powder
Purity: >99%
Size: 10mg
Contents: 5mg Tesamorelin/ 5mg CJC-1295
Form: Lyophilized powder
Purity: >99%
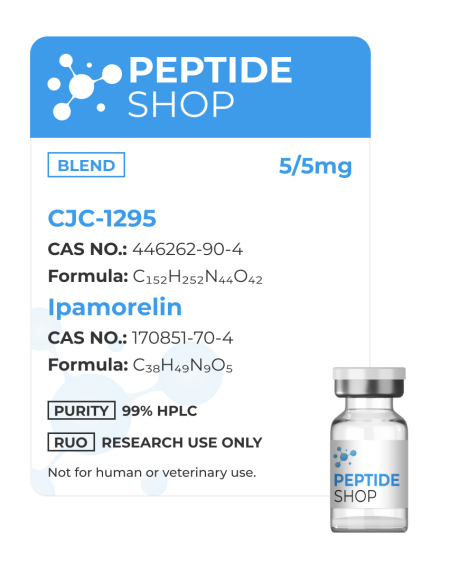
CJC-1295 and Ipamorelin peptide are often used in conjunction as their action is synergistic and more than doubly effective. PeptideShop.com offers this blend in a total quantity of 10mg (5mg each).
CJC-1295 Peptide
CJC-1295 is a synthetic hormone-releasing hormone analogue and growth hormone secretagogue. It was developed by ConjuChem Biotechnologies as a means to promote regulation and pulsatile GH secretion. GH therapy is an FDA approved way of treating its deficiencies, diseases such as Turner or Prader-Willi syndrome, idiopathic short stature etc.
The only problem with this approach to treatment is it might be problematic to determine the effectiveness of these therapies due to lacks of biological serum markers. CJC-1295 peptide was developed to mitigate these problems and uncover a more potent and measurable way of secreting GH without affecting its pulsatile nature.
Ipamorelin Peptide
Ipamorelin is also a growth hormone secretagogue, but it also acts as a ghrelin hormone secretagogue receptor agonist, as demonstrated in both in vitro and in vivo studies. Even though its effect is similar to that of CJC-1295, the interesting thing about Ipamorelin is that it does not raise ACTH (Adrenocorticotropic hormone), or cortisol levels for that matter, making it the first GHTP receptor agonist with selective GH release ability.
CJC-1295 And Ipamorelin Peptide Blend
Rather than administering one peptide or the other, more and more research is aimed at testing out the synergistic effect of these two peptides. Some studies showed a 3 or even 5 fold increase in growth hormone secretion increase!
Both CJC-1295 and Ipamorelin will stimulate the pituitary gland to increase GH production and release more hormones through the bloodstream. Animal studies also demonstrated significant ghrelin stimulation, resulting in food intake, fat deposition and muscle building control.
Despite seeing these beneficial results in both GH secretion and appetite regulation, this therapy is still not an FDA approved treatment, as most of our data comes from animal studies. Definitive human studies are needed before moving into the realm of human consumption.
References:

 Anti Aging
Anti Aging Hair Growth
Hair Growth Muscle Growth
Muscle Growth Peptide Blends
Peptide Blends Peptide Supplies
Peptide Supplies Peptides
Peptides Skin
Skin Testosterone
Testosterone Weight Loss
Weight Loss