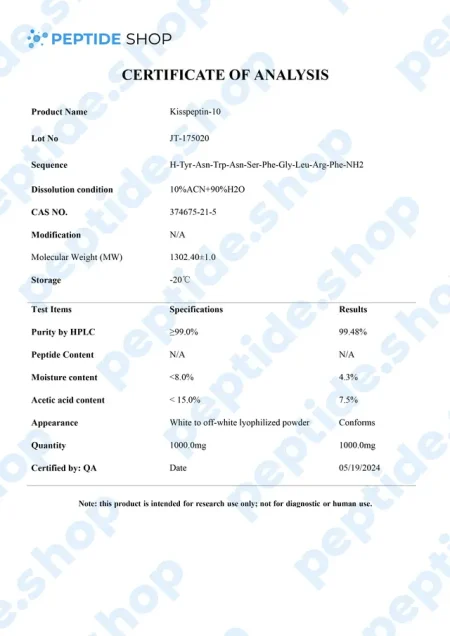
Kisspeptin 5mg/10mg
Metastin or Kisspeptin is believed to have the ability to prevent the spread of cancer or metastasis. This peptide is produced by the hypothalamus, which stimulates the release of GnRH or gonadotropin-releasing hormone, which then causes follicle-stimulating hormone and luteinizing hormone to be released from the purity gland.
Kisspeptin is used in testosterone replacement therapy instead of hCG to increase testosterone levels. That’s why it has emerged as a crucial regulator of the mammalian reproductive axis.
This peptide was first discovered in 1996 when it managed to inhibit melanoma cell lines. It belongs to a family of peptides that are derived from the KISS1/kiss1 gene structure, forming from prepro-kisspeptin, which has differential proteolysis for a common precursor.
Kisspeptin is classified as an RF or neuroactive peptide with a specific Arg-Phe-NH2 motif.
Benefits:
Kisspeptin binds to receptors in the pituitary gland, triggering a response that prompts the gland to release neurotransmitters, signaling the release of LH and FSH.
Based on numerous animal studies, scientists have managed to uncover the following benefits:
- Boosts the production of testosterone naturally
- Regulates fertility
- Increases sexual drive
- Improves immune response
- Boosts brain function
- Promotes weight loss
How does Kisspeptin work?
This peptide stimulates the release of GnRH or gonadotropin-releasing hormone. It enters the purity gland through receptor sites, causing a gland to release neurotransmitters, which later signal the releases of FH and LH. These hormones play a crucial role in the production of oestradiol and testosterone.
Kisspeptin mimics the action of hCG and clomiphene, and according to some animal studies, it can affect fertility in female and male animals.
Distribution of Kisspeptin
Kisspeptin was first found in the placenta, and later, it has been observed in the small intestine, pancreas, ovaries, and testis in mammals. The primary expression of Kisspeptin and its receptors have been shown in two big neuronal populations within the hypothalamus of rodents, the anteroventral periventricular nucleus and the arcuate nucleus.
$60.00 – $110.00
| Quantity: | 5mg, 10mg |
|---|---|
| Unit: | 1 vial |
| Contents: | Kisspeptin |
| Form/Appearance: | Lyophilized/Powder |
| Peptide Purity: | 99% |
| Sequence: | YNWNSFGLRF |
| Molecular Mass: | 1302.4 g/mol |
| Solubility: | Sterile / Bacteriostatic water |
| Synonyms: | KISS-1, Protein KISS-1, metastin, Kp-10 peptide |
Based on 0 reviews
|
|
|
0% |
|
|
|
0% |
|
|
|
0% |
|
|
|
0% |
|
|
|
0% |
FAQs
Related Products
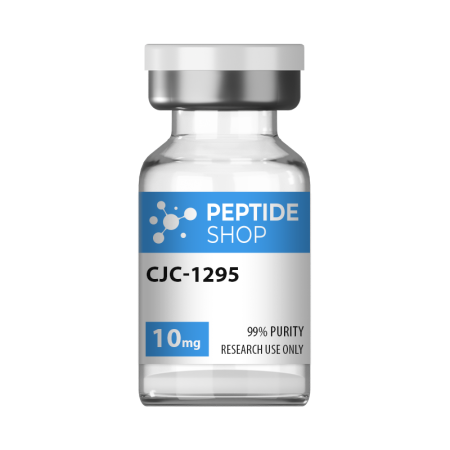
If you’re a peptide researcher (or plan on becoming one), you should know the difference between CJC-1295 and CJC-1295 DAC. CJC-1295 DAC features an additional component at the end of the peptide chain, also known as a drug affinity complex or DAC.
This small fragment changes the peptide’s functionality and extends its half-life to six to eight days. It might have a prolonged effect of up to two weeks.
Below, we will showcase the main similarities and differences between these two peptides, including their properties, characteristics, and mechanism of action.
What is CJC-1295 DAC peptide?
This peptide resembles the regular CJC-1925 since it is a modified form of natural GHGR (1-29). However, this one differs from CJC-1925. It has an additional molecule known as a “drug affinity complex.”
DAC features a couple of oxygen and nitrogen atoms connected by chemical bonds. According to some findings, this small number of atoms could significantly impact peptide breakdown rate and its use in the body.
What is CJC-1295 Peptide?
This peptide is also known as “modified growth hormone releasing factor (1-29)”, “ModGRF 1-29”, or “Modified GRF (1-29).” You may also encounter the name “CJC-1295, without DAC.”
All these names imply a specific peptide molecule containing a short amino acid chain. As many studies have indicated, this peptide may boost growth hormones in the bloodstream.
Growth hormone may have a significant role in several vital internal activities. It could facilitate cellular reproduction, repair, and growth, help with tissue repair, improve muscle cell development, support skin cells, and other functions.
While the body naturally produces growth hormone, this production tends to naturally decrease. According to some research done in laboratory settings, CJC-1295 may encourage the natural production of growth hormone, increasing its levels, which could lead to quicker repair, fat cell burn, and muscle cell growth.
Differences between CJC-1295 DAC and CJC-1295
As research studies have outlined, here are some fundamental differences between these two peptides.
Half-life
The main distinction lies in their half-lives. CJC-1295 is thought to mimic the body’s natural peptide. The endogenous GHRH has a short half-life of just a couple of minutes. Similarly, CJC-1295 has a brief half-life of around half an hour.
Regarding the second peptide, the additional DAC could significantly alter the organism’s peptide use. Researchers believe that DAC offers a peptide, a lysine linker, which could protect and prevent it from degrading.
Moreover, the DAC component could extend the half-life of this peptide to about six to eight days.
Properties of CJC-1295 DAC peptide
It is believed that CJC-1295 DAC boosts growth hormone levels in the bloodstream. Additionally, several studies suggest the following:
- Scientists and researchers need to focus their attention to studying the potential of growth hormones on growth and muscle recovery.
- Growth hormone may help convert fatty tissue into energy.
- Growth hormones are linked with collagen production in the skin, which means this peptide may also help with skin regeneration and skin cell development.
- CJC-1295 DAC may positively impact sleep patterns.
- Growth hormone is essential for tissue regeneration and helps the organism recover from damage.
References:
Teichman SL, Neale A, Lawrence B, Gagnon C, Castaigne JP, Frohman LA. Prolonged stimulation of growth hormone (GH) and insulin-like growth factor I secretion by CJC-1295, a long-acting analog of GH-releasing hormone, in healthy adults. J Clin Endocrinol Metab. 2006 Mar;91(3):799-805. doi: 10.1210/jc.2005-1536. Epub 2005 Dec 13. PMID: 16352683.
Sam L. Teichman, Ann Neale, Betty Lawrence, Catherine Gagnon, Jean-Paul Castaigne, Lawrence A. Frohman, Prolonged Stimulation of Growth Hormone (GH) and Insulin-Like Growth Factor I Secretion by CJC-1295, a Long-Acting Analog of GH-Releasing Hormone, in Healthy Adults, The Journal of Clinical Endocrinology & Metabolism, Volume 91, Issue 3, 1 March 2006, Pages 799–805,
American Journal of Physiology-Endocrinology and Metabolism 2006 291:6, E1290-E1294
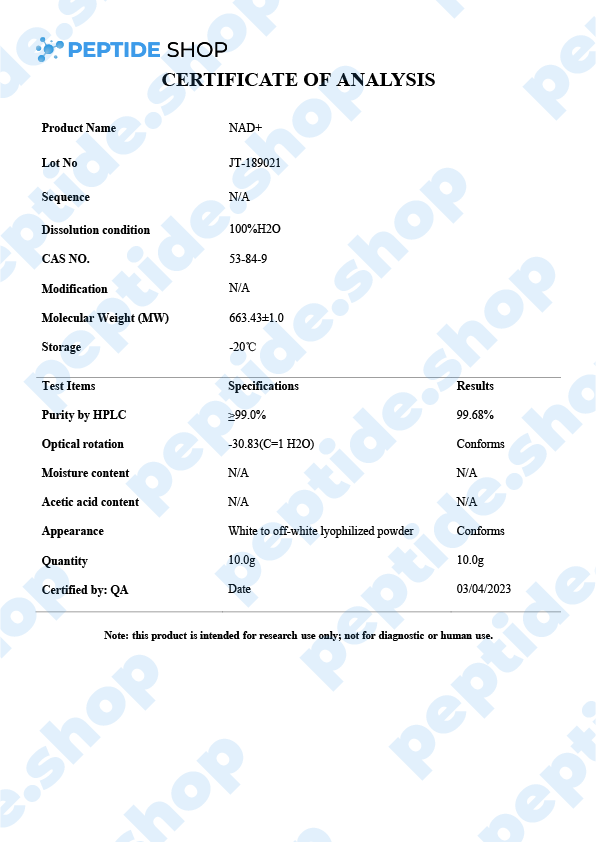
Nicotinamide adenine dinucleotide (NAD+) is a critical coenzyme that’s present in every living cell and, as such, is involved in a number of metabolic and cellular processes. This is why NAD+ is so interesting for many different areas of research such as:
- Anti aging
- Metabolic disorders
- Neurodegenerative disorders
- And even cancer research
PeptideShop.com sells NAD+ peptide in vials of 100mg and is meant for laboratory use only. Researchers commonly use it to test its effectiveness on:
- DNA damage repair and gene expression
- Stress response regulation
- Slowing down the progression of degenerative disorders
- Metabolism pathway testing
But, as previously mentioned, we are still waiting on large scale human tests.
NAD+ Role In Cellular Maintenance
Cellular NAD exists in two forms:
- NAD+
- NADH
When there’s a shift in NAD+ and its level drops in favor of NADH, this is a hallmark of aging; though the exact mechanisms that lead to this drop still remain unknown.
Naturally, numerous clinical studies showed that increasing NAD+ levels leads to the reduction of age-related immune and metabolic changes. Meaning there is potential of using NAD+ in treating age related disorders.
NAD+ And Neurodegenerative Disorders
When speaking about aging, one of the most contributing factors is mitochondrial dysfunction in neurons. Aging also speeds up the progression of neurodegenerative disorders, triggering DNA damage and mitochondrial impairment.
Luckily, studies have shown that NAD+ treatment (and even supplementation) helped restore mitochondrial function, enhance neural function and even improve cognitive abilities.
NAD+ And Metabolic Disorders
We’ve seen a dramatic increase in metabolic disorders lately, making it one of the major global health problems. Of course, we use the term metabolic disorders to cluster a whole host of problems such as obesity, diabetes, hypertension, as well as some cardiovascular pathologies.
NAD+ levels directly influence nutrient status in cells, so regulating them stands as a clear guideline to future research in hope of making NAD+ an FDA-approved way of treating metabolic and age related disorders.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7973386/
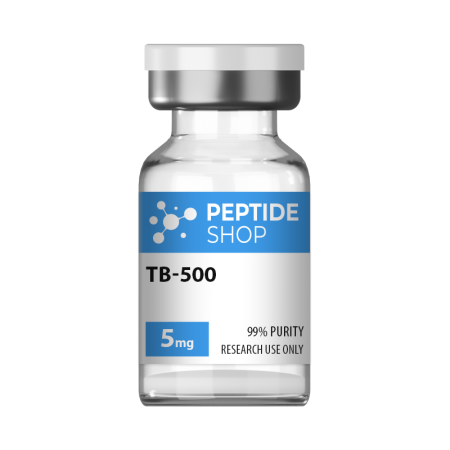
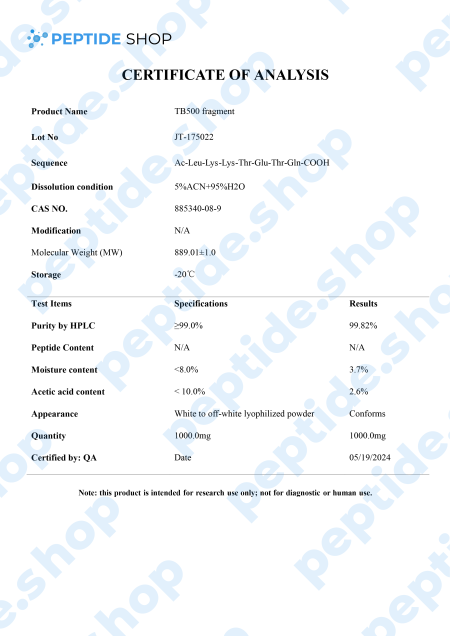
TB-500 is a 43 amino acid long synthetic peptide, analogue of thymosin beta-4. Thymosin beta-4 is a widely distributed peptide, and present in virtually all mammalian cells, which plays a pivotal role in many different processes in the body – it increases angiogenesis (formation of new blood vessels), proliferation, inhibits apoptosis (cell death) and inflammation.
Numerous animal clinical trials also showed that thymosin beta-4 can be used to indicate myocardial, liver and renal problems.
Angiogenesis:
Thymosin beta-4 promotes angiogenesis, triggers cell proliferation and migration, as well as the formation of capillary-like structures in cells. It also triggers blood perfusion (local fluid flow) by increasing capillary density.
Apoptosis:
Thymosin beta-4 inhibits apoptosis by inhibiting the transforming growth factor pathway. It also prevents nucleus pulposus (spinal disk providing shock absorption during movement) cell apoptosis and slows down cellular aging.
Inflammation:
In mouse models Tβ4 significantly dropped the number of inflammatory cells in the brains of the treated animals. It also prevented the production of proinflammatory cytokines and effectively blocked the increase of ethanol-induced inflammatory factors.
Heart Health:
Clinical data showed that thymosin beta-4 has a positive effect on both acute phase (immediately following the injury) where it preserves the ischemic myocardium, as well as in the chronic phase, in which it activates the growth of vascular cells.
After observing Tβ4’s benefits in animal models, it’s not surprising TB-500 gained so much popularity recently, since it acts as Tβ4’s synthetic analogue. Numerous clinical studies (in animal models) showed TB-500 as a potent way to improve blood vessel growth and fluid flow, accelerate wound healing, reduce oxidative stress and bind protein.
Of course, more research is needed to determine the full effects of this peptide, its safety and effectiveness in human test subjects.
Reference:
Xing Y, Ye Y, Zuo H, Li Y. Progress on the Function and Application of Thymosin β4. Front Endocrinol (Lausanne). 2021 Dec 21;12:767785. doi: 10.3389/fendo.2021.767785. PMID: 34992578; PMCID: PMC8724243.
CJC-1295 is a synthetic analogue of growth hormone-releasing hormone (GHRH) and growth hormone secretagogue (GHS) developed by ConjuChem Biotechnologies.
GHRH is a 44-amino acid long peptide which our hypothalamus synthesizes and in the pituitary gland, it binds to the growth hormone (GH) receptors, resulting in the release, regulation and pulsatile secretion of GH.
We already talked about GH therapy as being FDA approved in conditions such as GH deficiency, Turner syndrome, Prader-Willi syndrome, idiopathic short stature etc. Recombinant human GH treatment is generally performed as one daily, subcutaneous injection which elevates the levels of GH serum in the blood.
One of the major problems with this approach to treatment is that the efficacy of GH therapy is hard to determine due to the lack of biological serum biomarkers. Currently, most facilities are using levels of IGF-1 and IGFBP-3 to monitor the efficacy of this therapy but these levels may vary wildly (due to growth velocity, glucose tolerance, insulin levels etc.).
Furthermore, GH abuse extended across multiple sports disciplines, making it even harder to suppress and put this problem under control.
Researchers hope to solve this problem by employing new biomarkers of GH action and secretion. One such way is to employ newly developed molecules, such as CJC-1295, shown to increase both GH and IGF-1 levels in the blood, without affecting the pulsatility of GH secretion. CJC-1295 also has a prolonged half-life of 8 to 10 days, due to its ability to bind to the endogenous serum albumin.
So, what scientists are hoping to achieve with CJC-1295 is both a safe way of promoting GH secretion as well as making it measurable in a laboratory setting. There were numerous studies tackling this issue, but we still need further testing to confirm these preliminary findings.
Reference:
Sackmann-Sala L, Ding J, Frohman LA, Kopchick JJ. Activation of the GH/IGF-1 axis by CJC-1295, a long-acting GHRH analog, results in serum protein profile changes in normal adult subjects. Growth Horm IGF Res. 2009 Dec;19(6):471-7. doi: 10.1016/j.ghir.2009.03.001. Epub 2009 Apr 21. PMID: 19386527; PMCID: PMC2787983.
Melanotan 2 is a synthetic version of human alpha-melanocyte stimulating hormone and acts as a non selective melanocortin-receptor agonist. It was mainly developed as a sunless tanning option, but some clinical studies showed it also causes spontaneous penile erections, as well as general sexual stimulation.
Some of the other “side effects” researchers noticed were reduction in compulsive behavior, reduced glucagon production, hunger suppression and even some limited addiction control.
Melanotan 2 Effects On Autism
There is some additional recent clinical research suggesting there might be a link between Mealnotan 2 and autism. Of course, melanotan treatment cannot reverse autism, sadly, but it may act on some aspects of this disorder and make it more manageable.
In mouse model studies researchers recorded that MT2 stimulated oxytocin release, which had the potential to reduce (in some cases counteract) common ASD behaviors – behaviors that include:
- Hand clapping
- Bouncing on toes
- Body rocking
- Holding body parts in unusual positions
- Repeating vocalizations etc.
Obesity’s become a global pandemic, currently affecting one third of the entire population, and this is why we can look at it as a chronic disease that requires appropriate treatment.
When talking about obesity, amylin hormone is of great importance as it gets secreted along with insulin and acts as food intake inhibitor, delaying gastric emptying and suppresses post-prandial glucagon responses to meals.
For this reason, there is a tendency to include amylin management in newly developed medication.
And one such compound is cagrilintide – lipidated long-acting amylin analogue.
Though it still hadn’t been thoroughly tested on humans, numerous rat studies showed incredible potential. One such in vitro study involving rats set out to compare cagrilintide’s effectiveness against pramlintide (an FDA-approved diabetes 1/2 medication).
The study showed that pramlintide reduced food intake by 25% in the period of 0-24 hours (it did not cause reduced food intake after 24 hours). But the dosage was substantial – 1000 nmol/kg.
On the other hand, cagrilintide was able to reduce food intake by approximately 50% with a minimal dosage of only 3 nmol/kg. More importantly, this food intake reduction spanned across 60 hours from the moment it was injected.
These results clearly show the potency of cagrilintide in weight loss and diabetes management medication, especially because it acts over such a long time period (allowing subcutaneous injections to be applied once a week).
Reference:
Dehestani B, Stratford NR, le Roux CW. Amylin as a Future Obesity Treatment. J Obes Metab Syndr. 2021 Dec 30;30(4):320-325. doi: 10.7570/jomes21071. PMID: 34929674; PMCID: PMC8735818.
Growth hormone replacement therapy has long been accepted as one of the most effective ways of treating GH deficiency and related conditions. This therapy uses recombinant human growth hormone (rhGH) and, despite its longstanding usage record, it has been surrounded by controversy. Even though, in the short term, this therapy is very effective, when it comes to long term effects, issues start to arise:
- Long term improper dosage can lead to some severe side effects
- This therapy may affect normal physiology after prolonged application
- Some federal regulations might interfere with the therapy
- There’s even some concerns that this therapy may awaken latent cancers and cause metabolic disorders
There is one more major problem with dosage because the body can’t properly modulate tissue exposure to rhGH. Meaning, the practitioner uses their “best guess” to access the appropriate dosage.
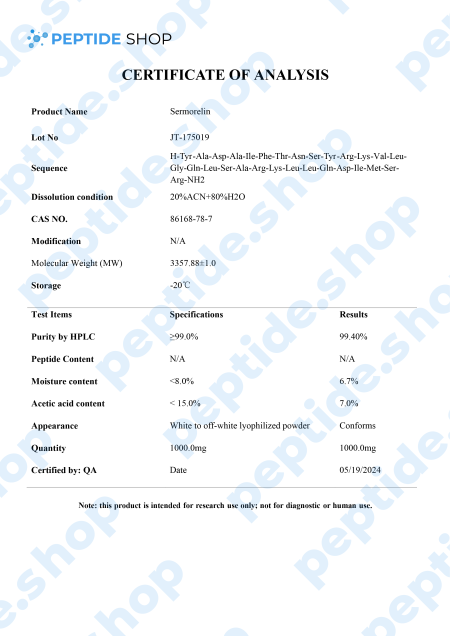
This is why researchers are looking for alternative ways to stimulate GH production by targeting GH secretagogues and promoting pituitary gland health. One such molecule is sermorelin, a GHRH analog that impacts the hypothalamic-pituitary-pituitary-somatotropic axis.
It’s used for both treatment and diagnosis of GH deficiency as research studies showed sermorelin promoted change in GH levels similar to those observed with endogenous GHRH. It also stimulates FSH (follicle-stimulating hormone) and LH (luteinizing hormone), which implies a potential role in the treatment of hypogonadism.
Though we need larger, longitudinal studies, sermorelin proved as a promising GH and IGF-1 stimulator and diagnostic agent.
Reference:
Walker RF. Sermorelin: a better approach to management of adult-onset growth hormone insufficiency? Clin Interv Aging. 2006;1(4):307-8. doi: 10.2147/ciia.2006.1.4.307. PMID: 18046908; PMCID: PMC2699646.
Sinha DK, Balasubramanian A, Tatem AJ, Rivera-Mirabal J, Yu J, Kovac J, Pastuszak AW, Lipshultz LI. Beyond the androgen receptor: the role of growth hormone secretagogues in the modern management of body composition in hypogonadal males. Transl Androl Urol. 2020 Mar;9(Suppl 2):S149-S159. doi: 10.21037/tau.2019.11.30. PMID: 32257855; PMCID: PMC7108996.
Semax is an interesting nootropic that can capture the attention of researchers, health professionals, and enthusiasts alike. It was originally developed in Russia back in the 1980s and 1990s. Nowadays, Semax is believed to enhance a range of cognitive and neuroprotective properties.
Many know this peptide by its trade name, such as Semaxum, and it has been extensively researched by institutions such as the Institute of Molecular Genetics of the Russian Academy of Science.
What is Semax?
Semax is a peptide best known for its neurogenic, neuroprotective, and nootropic properties. It was developed based on the molecular structure of ACTH or adrenocorticotropic hormone. Preliminary studies in small-scale human trials, animals, and cells indicate potential benefits of Semax use.
In the U.S. and multiple countries around the world, this component is the basis for a number of medicines that are used in clinical practices for the treatment of optic nerve atrophy, dys-circulatory encephalopathy, and ischemic brain stroke.
Potential benefits
Some of the benefits Semax may include:
- Increased short-term memory and attention
- Better non-proliferative diabetic neuropathy
- Can assist during recovery from hypoxia/stroke
- Can help with glaucoma optic neuropathy
- May act as an analgesic
- It may help in treating ADHD
- It may help protect the brain from various types of damage and stress
How Does Semax Work?
Semax increases BDNF or brain-derived neurotrophic factor. BDNF is one of the most active neurotrophins, which help control and stimulate neurogenesis, creating new neurons in the brain. This component helps support neuroplasticity, allowing nerve cells in the brain to adapt to new situations and recover from injury.
Additionally, BDNF encourages the survival of existing neurons and supports the growth, creation, and regeneration of new synapses and neurons.
This nootropic also helps minimize the breakdown of enkephalins. Enkephalins are mostly involved in reducing inflammation, decreasing pain, boosting immune cell activity, and preventing cancer cell growth.
They also play a role in pain, emotional behavior, learning, and memory. Balanced enkephalins are necessary to maintain normal brain function. Therefore, researchers are led to believe that Semax may potentially relieve pain. However, more research is needed to confirm the preliminary findings.
References:
Medvedeva EV, Dmitrieva VG, Povarova OV, Limborska SA, Skvortsova VI, Myasoedov NF, Dergunova LV. The peptide semax affects the expression of genes related to the immune and vascular systems in rat brain focal ischemia: genome-wide transcriptional analysis. BMC Genomics. 2014 Mar 24;15:228. doi: 10.1186/1471-2164-15-228. PMID: 24661604; PMCID: PMC3987924.
https://www.sciencedirect.com/science/article/abs/pii/S0306987706005391
Gusev, E. & Martinov, Michail & Kostenko, E. & Petrova, Lyudmila & Bobyreva, S.. (2018). The efficacy of semax in the tretament of patients at different stages of ischemic stroke. Zhurnal nevrologii i psikhiatrii im. S.S. Korsakova. 118. 61. 10.17116/jnevro20181183261-68.
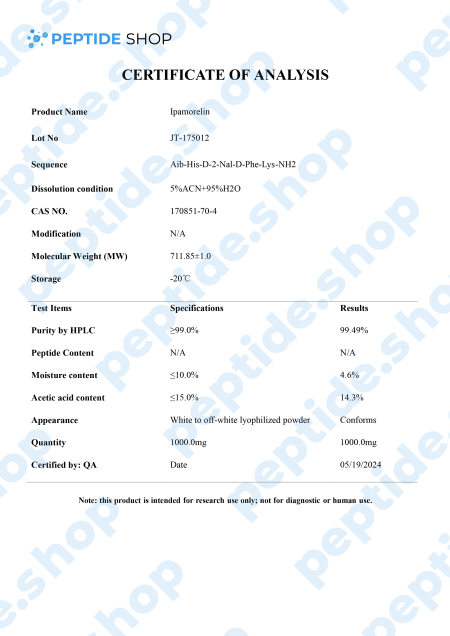
Ipamorelin is a pentapeptide that showed a significant growth hormone secretion potential both in vitro and in vivo studies. In vivo studies, it showed a similar potency and effectiveness as GHRP-6 (a synthetic growth hormone-releasing hexapeptide) as it stimulates GH release via the GHRP receptors.
What’s interesting about ipamorelin is that it did not raise ACTH (Adrenocorticotropic hormone) nor cortisol level significantly; something we’ve seen happening with GHRP-6 and GHRP-2. So, we can conclude that ipamorelin is the first GHRP-receptor agonist with GH release selectivity similar to GHRH. This is why ipamorelin is an interesting candidate for further testing.
In addition to stimulating GH secretion, this peptide has seen some interesting use in the treatment of postoperative ileus (POI), a condition characterized by transient loss of gastrointestinal motility following abdominal surgery.
The exact mechanism behind POI is a complex one, involving many different bodily structures; in addition, condition is often worsen due to the opioid drugs used for patient pain management.
In rodent studies, ipamorelin was found to selectively stimulate ghrelin (hormone produced by our stomach, affecting food intake, deposition and growth hormone release) without raising cortisol or adrenocorticotropic hormone levels. These effects were shown in both lower GI tract as well as the upper, making this peptide a viable candidate for potential POI treatment.
References:
Raun K, Hansen BS, Johansen NL, Thøgersen H, Madsen K, Ankersen M, Andersen PH. Ipamorelin, the first selective growth hormone secretagogue. Eur J Endocrinol. 1998 Nov;139(5):552-61. doi: 10.1530/eje.0.1390552. PMID: 9849822.
Greenwood-Van Meerveld B, Tyler K, Mohammadi E, Pietra C. Efficacy of ipamorelin, a ghrelin mimetic, on gastric dysmotility in a rodent model of postoperative ileus. J Exp Pharmacol. 2012 Oct 19;4:149-55. doi: 10.2147/JEP.S35396. PMID: 27186127; PMCID: PMC4863553.
Numerous studies have shown that this peptide may represent numerous opportunities for competent scientists to investigate, especially cartilage regeneration and fatty tissue mitigation.
What is Fragment 176-191 peptide?
This synthetic amino acid sequence mimics the hGH sequence, starting from position 177 to position 191.
AOD 9604, or “lipolytic extract,” is another name for Fragment 176-191. Many researchers argue that Fragment 177-191 may be an important research compound in the context of obesity. They believe it can potentially burn fat in animal models in laboratory settings.
Despite positive results, Fragment 176-191 hasn’t been used for human research purposes and doesn’t have official medical approvals.
Growth hormone
According to research, it appears that hGH Fragment 176-191 may not produce any side effects often related to hGH supplementation. Several adverse effects, such as, impaired glucose tolerance, insulin resistance, and increases in IGF-a levels, have cast doubt on hGH’s use as an obesity treatment. However, when it comes to hGH Fragment 176-191, it doesn’t seem to be impacting blood IGF-1 levels or negatively affecting carbohydrate metabolism.
A trial conducted on Zucker rats in 2000 showed no detrimental effects on insulin sensitivity. Also, an investigation on obese mice done in 2001 did not seem to affect insulin secretion.
Properties
Studies conducted on animals suggest that this peptide can exhibit significant theoretical properties, which will be outlined below:
- The main potential of this Fragment is its lipolytic properties or, in other words, fat-reducing potential. While growth hormones promote development in infancy, they have also been speculated to have an important purpose in maturity.
- Lipoprotein lipase inhibitors may be activated in fat cells,
- By stimulating lipolysis in adipocytes may lead to a decrease in fat cell bulk,
- It might lead to loss of fat from the host body,
Weight
A 14-day trial researching overweight mice came to a conclusion that Fragment 176-191 may have increased skeletal muscle thermogenesis and boosted fat burning.
The study results indicated that this peptide may have enhanced beta (3)-AR RNA (ADRB3) levels, which caused rapid weight reduction in overweight animals but didn’t have much effect on lean mice.
Cartilage
Based on other animal research, it appears that hGH Fragment 176-191 may boost the effects of hyaluronic acid (HA). When Fragment 176-191 was combined with hyaluronic acid, it might boost cartilage formation in white rabbits which have issues with osteoporosis.
References:
Habibullah MM, Mohan S, Syed NK, Makeen HA, Jamal QMS, Alothaid H, Bantun F, Alhazmi A, Hakamy A, Kaabi YA, Samlan G, Lohani M, Thangavel N, Al-Kasim MA. Human Growth Hormone Fragment 176-191 Peptide Enhances the Toxicity of Doxorubicin-Loaded Chitosan Nanoparticles Against MCF-7 Breast Cancer Cells. Drug Des Devel Ther. 2022 Jun 27;16:1963-1974. doi: 10.2147/DDDT.S367586. PMID: 35783198; PMCID: PMC9249349.
https://www.sciencedirect.com/science/article/abs/pii/0304416582900332
Habibullah, Mahmoud & Mohan, Syam & Syed, Nabeel & Makeen, Hafiz & Jamal, Qazi & Alothaid, Hani & Bantun, Farkad & Hakamy, Ali & Kaabi, Yahia & Samlan, Ghalia & Lohani, Mohtashim & Thangavel, Neelaveni & Al-Kasim, Mohamed. (2022). Human Growth Hormone Fragment 176–191 Peptide Enhances the Toxicity of Doxorubicin-Loaded Chitosan Nanoparticles Against MCF-7 Breast Cancer Cells. Drug Design, Development and Therapy. 16. 1963. 10.2147/DDDT.S367586.
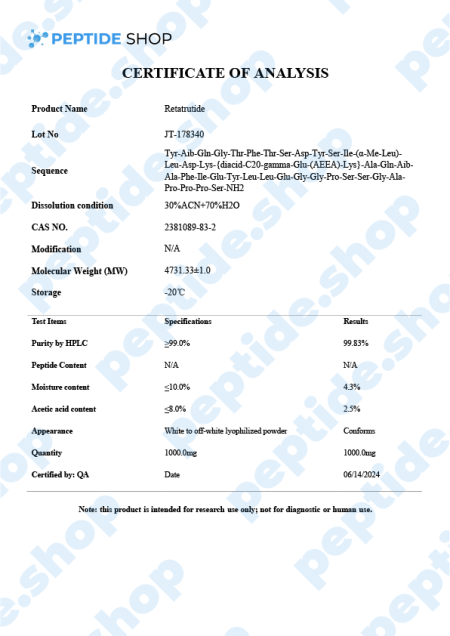
Retatrutide is one of the latest incretin mimetic drugs being tested for their weight reduction properties. Researchers use incretin mimetic agents as they work to mimic incretin hormones (gut peptides that get secreted after we eat) to allow for a better insulin secretion and hyperglycaemic control.
Even though there are numerous weight reduction agents being prescribed and used, FDA-recognized “treatment” for nonsyndromic obesity are:
- Orlistat
- Phentermine-topiramate
- Naltrexone‐bupropion
- Liraglutide and
- Semaglutide
With the exception of glucagon-like peptide 1 receptor agonists (such as semaglutide), most weight reduction agents come with a specific set of side effects such as nausea, gastrointestinal distress, abdominal pain, vomiting, diarrhea, or a general weight decrease that does not cross the 15% mark. Some of these medications even come with a warning against using them if a patient is suffering from a kidney, heart, thyroid or any related problems.
This is why scientists are turning more and more to retatrutide, because this incretin mimetic decreases appetite, promotes the feeling of fullness and slows down the process of gastric emptying, but does all that while presenting with minimal side effects and increased weight loss effectiveness, compared to liraglutide or semaglutide.
Retatrutide Mechanism of Action
Retatrutide exerts a powerful glucagon-receptor agonistic effect. When we compare it to human glucagon and glucagon-like peptide 1 (GLP-1), it exhibits:
- Reduced potency on the GCGR (human glucagon receptor) and GLP-1R (glucagon-like peptide-1 receptor)
- Enhanced potency at the human GIPR (gastric inhibitory polypeptide receptor)
When talking about in vitro experiments, retatrutide demonstrated similar efficacy in evoking glucose production within hepatocytes and inducing lipolysis. Also, retatrutide showed a favorable half-life of 6 days, enabling it a weekly dosage regimen (should the drug get FDA approved).
Another double-blind study conducted in the US on obese patients showed promising results. 338 adults in total were involved, split into 6 cohorts (depending on the weekly dosage), up against a placebo group. Retatritude group experienced the following results:
- 1mg group – after 24 weeks this group experienced weight loss of 7.2%, and after 48 weeks a total loss of 8.7%
- 4mg group (commencing with 2mg) – after 24 weeks this group experienced a weight loss of 11.8%, and after 48 weeks a total loss of 16.3%
- 4mg group (commencing with 4mg) – after 24 weeks this group experienced a weight loss of 13.9%, and after 48 weeks a total loss of 17.8%
- 8mg group (commencing with 2mg) – after 24 weeks this group experienced a weight loss of 16.7%, and after 48 weeks a total loss of 21.7%
- 8mg group (commencing with 4mg) – after 24 weeks this group experienced a weight loss of 17.9%, and after 48 weeks a total loss of 23.9%
- 12mg group (commencing with 2mg) – after 24 weeks this group experienced a weight loss of 17.5%, and after 48 weeks a total loss of 24.2%
In contrast, the placebo group only experienced a 1.6% weight loss after 24 weeks and 2.1% after 48. Findings also showed that adverse effects related to retratitude treatment (such as nausea, vomiting, diarrhea and constipation), were mild and depended on the dosage.
In conclusion, this peptide showed promising results in addressing obesity in both in vitro and human test subject studies. However, test samples were relatively small, and we still need more research and clinical trials to show the effectiveness of retratutide as an effective, long-term way of managing weight.
Reference:
Naeem M, Imran L, Banatwala UESS. Unleashing the power of retatrutide: A possible triumph over obesity and overweight: A correspondence. Health Sci Rep. 2024 Feb 5;7(2):e1864. doi: 10.1002/hsr2.1864. PMID: 38323122; PMCID: PMC10844714.
Hunger and satiety signals are controlled by serotonin, dopamine, norepinephrine and a number of other systems within our body. When talking about weight loss and appetite modulation, there are agents that do it through pure central nervous system pathways, and those that target peripheral signals (that travel to the central nervous system).
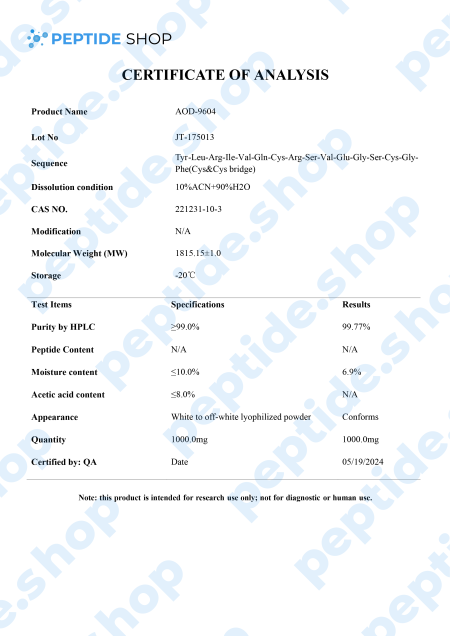
This is why we have so many different weight loss options, since medication is based on substances affecting different pathways, signals and weight management systems. One such drug, aimed at improving adipose tissue function and fatty acid metabolism is AOD9604.
AOD9604 is a modified form of human growth hormone fragment 176-191, developed to stimulate prolipid mobilizing and lipid oxidation (during which fatty acids decompose into carbonyl compounds, unsaturated aldehydes, ketones and other substances).
Even though AOD9604 has not yet been deemed FDA-approved,a number of studies showed its administration led to a significant weight loss and improvements in glucose tolerance (in both animal and early stage human studies).
Another such study done on 300 obese individuals in Australia showed that AOD9064 administration more than tripled weight loss in test subjects, compared to those on a placebo drug. Furthermore, this study proved that long-term treatment is not likely to cause resistance to AOD9064 based medication, making it a perfect candidate for future weight loss medication and treatment.
So far, animal and human studies both showed AOD9064’s effectiveness in helping test subjects lose weight, improve glucose tolerance, while presenting with minimal side effects. Further research studies are needed before including it into an FDA-approved treatment procedure, but the initial findings show a great potential.
Reference:
Michael D. Jensen. Potential Role of New Therapies in Modifying Cardiovascular Risk in Overweight Patients with Metabolic Risk Factors. 06 September 2012


 Anti Aging
Anti Aging Hair Growth
Hair Growth Muscle Growth
Muscle Growth Peptide Blends
Peptide Blends Peptide Supplies
Peptide Supplies Peptides
Peptides Skin
Skin Testosterone
Testosterone Weight Loss
Weight Loss








Reviews
There are no reviews yet.