Cerebrolysin 2mg, 5mg
Cerebrolysin is a porcine-derived peptide preparation, with a low molecular mass and a variety of research applications. An interesting thing about cerebrolysin is that its preparation contains nerve growth factors, BDFN (brain derived neurotrophic factor), Ciliary nerve growth factor, p-21 and orexin. This means that cerebrolysin contains molecules with:
- Pharmacodynamic properties – it expresses biochemical, physiological and molecular effects within the body.
- Neurotrophic properties – it aids in growing, repair and neuron maintenance
- Neuroprotective properties – it strengthens the neural pathways as well as the neurons themselves and improves synaptic plasticity.
Cerebrolysin Chemical Structure
It’s a bit difficult talking about cerebrolysin as it does not have a single chemical structure, rather, it’s a combination of several different peptides. As such, cerebrolysin is actually labeled an “orphan drug” by the FDA. What this means is it did show promise in disease treatment and prevention (in clinical trials), but only in orphan diseases. Orphan disease is one that affects fewer than 200,000 people in the US. This is why this peptide mix is not a profitable venture for further, independent studies, and research is only possible with financial help from the government.
But in the particular case of cerebrolysin, the government did, in fact, intervene, due to its potential in dealing with dementia and because of its neuroprotective capabilities.
This peptide mix was first developed in Austria, back in 1940 and has since become a vital medicine in Asia, especially Russia and China. Research studies showed that it has the ability to cross the blood-brain barrier and express its pharmacodynamic effects on both brain and the spinal cord.
But, what does it do?
Since cerebrolysin is not a single chemical compound, as we already said, we can look at it, and its effects, through the components its made of:
- Brain-Derived Neurotrophic Factor (BDNF) – this is a protein found in our central nervous system, shown to have a profound effect on neuron growth, synapse growth and health. Research in depression and Alcheimer’s disease revealed disrupted BDNF pattern expression.
- Glial Cell Line-Derived Neurotrophic Factor (GCNF) – this is an exceptionally important, naturally occurring peptide that promotes neuron survival, decreases the loss of neurons and, as some studies have pointed out, has the potential to aid the prevention of Parkinson’s and ALS.
- Ciliary Neurotrophic Factor (CNTF) – this is an interesting hormone affecting the growth of certain neural cells and has been a subject of numerous trials aimed at treating ALS.
- Nerve Growth Factor (NGF) – this is a particularly important peptide which regulates the growth, survival and neuron increase in number. Some studies showed NGF is one of the important factors in programmed cell death and regulation of certain immune system mechanisms.
Looking at these effects, it’s not hard to imagine why scientists used these molecules – to try and merge all these positive effects into one single mix. But were they successful? We actually have some clinical trials atesting to these possibilities:
- Cerebrolysin and Dementia – a study done in 2012 evaluated the outcomes of cerebrolysin therapy in patients with Alcheimer’s over the course of a 12 week treatment period. The study showed significant improvements in cognitive functions and the symptoms of dementia lasting up to several months after the study was finished.
- Cerebrolysin and Parkinson’s – we know that the onset of Parkinson’s disease has to do with the protection of dopamine producing neurons. The loss of these neurons is what leads to motor deficits characteristic for this disease. Unfortunately, we haven’t had human trials, but the one on mice showed that cerebrolysin administration protected these neurons and also lowered certain hormones responsible for Parkinson’s disease worsening.
- Stroke and Brain Injuries – though we don’t have many studies dealing with this topic, some small-scale ones showed cerebrolysin as being not only safe to use, but also helpful in recovery rate if given within 72 hours. Research in infants with brain injury induced communication delay also showed cerebrolysin improved therapeutic outcomes.
Even though these positive effects may seem overwhelming, leaving you wondering why cerebrolysin is not a mainstream, FDA-approved drug still, it’s important to note most of these findings were done on a limited sample (and mostly on animal studies). We have yet to see its effects in large-scale studies and, more importantly, see the long-term benefits of cerebrolysin therapy. Even though the initial results seem promising, we need to be patient and wait for more information before the final verdict.
References:
https://gsrs.ncats.nih.gov/ginas/app/beta/substances/37KZM6S21G%20
Allegri RF, Guekht A. Cerebrolysin improves symptoms and delays progression in patients with Alzheimer’s disease and vascular dementia. Drugs Today (Barc). 2012 Apr;48 Suppl A:25-41. doi: 10.1358/dot.2012.48(Suppl.A).1739721. PMID: 22514793.
Plosker GL, Gauthier S. Cerebrolysin: a review of its use in dementia. Drugs Aging. 2009;26(11):893-915. doi: 10.2165/11203320-000000000-00000. PMID: 19848437.
Masliah E, Armasolo F, Veinbergs I, Mallory M, Samuel W. Cerebrolysin ameliorates performance deficits, and neuronal damage in apolipoprotein E-deficient mice. Pharmacol Biochem Behav. 1999 Feb;62(2):239-45. doi: 10.1016/s0091-3057(98)00144-0. PMID: 9972690.
Ozkizilcik A, Sharma A, Lafuente JV, Muresanu DF, Castellani RJ, Nozari A, Tian ZR, Mössler H, Sharma HS. Nanodelivery of cerebrolysin reduces pathophysiology of Parkinson’s disease. Prog Brain Res. 2019;245:201-246. doi: 10.1016/bs.pbr.2019.03.014. Epub 2019 Apr 2. PMID: 30961868.
Ozkizilcik A, Sharma A, Lafuente JV, Muresanu DF, Castellani RJ, Nozari A, Tian ZR, Mössler H, Sharma HS. Nanodelivery of cerebrolysin reduces pathophysiology of Parkinson’s disease. Prog Brain Res. 2019;245:201-246. doi: 10.1016/bs.pbr.2019.03.014. Epub 2019 Apr 2. PMID: 30961868.
Hassanein SM, Deifalla SM, El-Houssinie M, Mokbel SA. Safety and Efficacy of Cerebrolysin in Infants with Communication Defects due to Severe Perinatal Brain Insult: A Randomized Controlled Clinical Trial. J Clin Neurol. 2016 Jan;12(1):79-84. doi: 10.3988/jcn.2016.12.1.79. Epub 2015 Sep 11. PMID: 26365023; PMCID: PMC4712290.
$50.00 – $110.00
| Quantity: | 2mg, 5mg |
|---|---|
| Unit: | 1 vial |
| Contents: | Cerebrolysin |
| Form/Appearance: | Lyophilized/Powder |
| Peptide Purity: | 99% |
| Sequence: | / |
| Molecular Mass: | / |
| Solubility: | Sterile / Bacteriostatic water |
| Synonyms: | Pitocin, Endopituitrina, Ocytocin |
Based on 0 reviews
|
|
|
0% |
|
|
|
0% |
|
|
|
0% |
|
|
|
0% |
|
|
|
0% |
FAQs
Related Products
Epitalon is a synthetic peptide, made up of 4 amino acids – alanine, glycine, glutamic and aspartic acid. It’s based on a natural peptide epithalamion, commonly extracted from the pineal gland. Some earlier studies showed epitalon’s antioxidant potential, so more recent ones started focusing on its anti-aging potential.
Recent studies also showed its potential in regulating DNA changes, treating infectious diseases… even addressing some types of cancer.
Anti Aging Properties
The fact that epitalon is epithalamin’s extract, means it has the ability to eliminate free radicals that cause tissue damage. A particular research study on flies and mice showed that, after epitalon’s administration, fruit flies mortality rate dropped by a whopping 52%, while the mortality rate in rats dropped by 27%, as compared to the control studies. What researchers learned from this study was that regular epitalon administration stimulated the synthesis and secretion of melatonin, which inhibits free radical production and its subsequent damage.
There was another in vitro study on human somatic non-reproductive cells suggesting that epitalon peptide affects telomerase activity. Telomerase is an enzyme present in cells, allowing them to live longer. So, essentially, this study showed the researchers that this therapy leads to the prolonged cell lifespan. Of course, we still need full scale human studies to see the full extent of prolonged cell lifespan.
DNA Effects
Epitalon also interacts with DNA gene expression, allowing it to have an indirect effect on a whole host of potential bodily functions – from immune system, to skin, tendon and connective tissue repair.
This essentially allows epitalon peptide therapy to have a dual potential effect – on the one hand, it strengthens the immune system and protects the body from outside factors, and on the other, it allows the body to repair and regenerate its structures on its own.
Skin Cell Regeneration
We already talked about epitalon’s effect on DNA and genes. This effect extends to the fibroblast producing and maintaining MMP2. Interestingly, this peptide also affects other skin components, such as collagen and elastin.
Of course, we still have yet to see definitive human studies, but animal ones showed promising results. Young and old rats exposed to epitalon showed skin fibroblast proliferation of 29 and up to 45%. Not only that, epitalon also activates enzymes that slow down programmed cell death.
References:
Yue X, Liu SL, Guo JN, Meng TG, Zhang XR, Li HX, Song CY, Wang ZB, Schatten H, Sun QY, Guo XP. Epitalon protects against post-ovulatory aging-related damage of mouse oocytes in vitro. Aging (Albany NY). 2022 Apr 12;14(7):3191-3202. doi: 10.18632/aging.204007. Epub 2022 Apr 12. PMID: 35413689; PMCID: PMC9037278.
Anisimov VN, Mylnikov SV, Khavinson VK. Pineal peptide preparation epithalamin increases the lifespan of fruit flies, mice and rats. Mech Ageing Dev. 1998 Jun 15;103(2):123-32. doi: 10.1016/s0047-6374(98)00034-7. PMID: 9701766.
Khavinson VKh, Bondarev IE, Butyugov AA. Epithalon peptide induces telomerase activity and telomere elongation in human somatic cells. Bull Exp Biol Med. 2003 Jun;135(6):590-2. doi: 10.1023/a:1025493705728. PMID: 12937682.
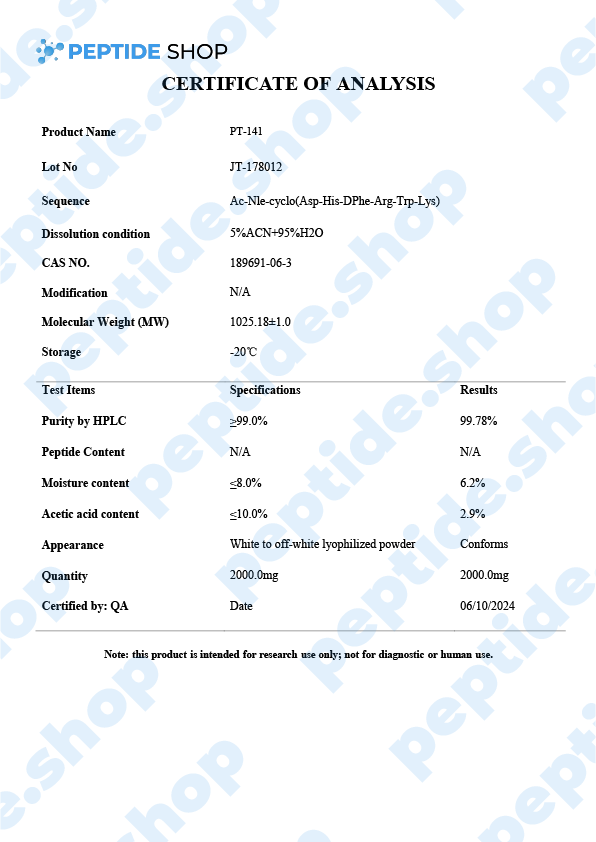
Also called Bremelanotide, PT-141 is a synthetic melanocortin receptor agonist that promotes dopamine release. Since it has such a high affinity for MC4R (Melanocortin 4 Receptor), in the presynaptic neurons of the hypothalamus, it has been approved as a treatment for HSDD (hypoactive sexual desire disorder) in premenopausal women. Under the brand name Vyleesi, Bremelanotide is the first and only FDA-approved way of HSDD treatment.
Sexual Dysfunctions
As we already said, PT-141 is an effective treatment for HSDD in premenopausal women but it’s important to note it should not be used as a treatment in women who already went through menopause or as a way of boosting sexual performance in men. These have not yet been fully tested.
We’ve seen the effectiveness of PT-141 (Bremelanotide) demonstrated in numerous studies. One such study followed female test subjects over the course of 52 weeks where the treated group received a 1.75mg dose right before anticipated sexual intercourse. All participants showed higher scores on general arousal, desire and orgasm, as compared to the placebo group. Also, no major side effects were linked to PT-141 application – the “most severe” ones were nausea, flushing and headache, which only occurred in around 10% of the participants.
Interestingly enough, scientists are still unsure about the Bremelanotide’s exact mechanism of action and how it leads to increased sexual desire in female patients. All we know is that it’s a potent alpha melanocyte-stimulating hormone, binding predominantly to the receptors MC4R and MC1R, and, to a certain extent, to MC1R-MC5R.
PT-141 And Erectile Dysfunction
At the beginning of the article we said that PT-141 (bremelanotide) should not be used to increase sexual desire in men… but this is not entirely true as there is some emerging evidence that this peptide does affect male sexual performance.
Currently, there are a number of effective ED treatment options available. One of the most fail-proof and common ones, incidentally the most invasive one, is an intracavernosal injection – where an injection is applied directly to corpus cavernosum (spongy tissue that runs through the shaft of the penis).
Naturally, researchers are on the lookout for a new, less invasive treatment option and are testing PT-141 as such. Though research is still in its early stages, results showed significant increases in both duration and the erection quality in both “regular” men, as well as those known to be taking viagra.
We still need more research to confirm all these findings and determine the safety and efficacy of using PT-14 as a reliable ED treatment option, but clinical studies suggest we are heading in this direction.
https://www.sciencedirect.com/topics/medicine-and-dentistry/bremelanotide
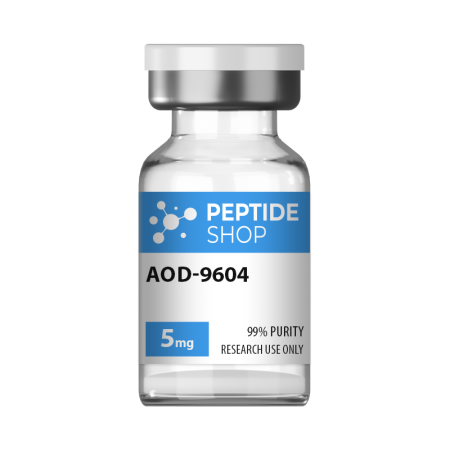
Hunger and satiety signals are controlled by serotonin, dopamine, norepinephrine and a number of other systems within our body. When talking about weight loss and appetite modulation, there are agents that do it through pure central nervous system pathways, and those that target peripheral signals (that travel to the central nervous system).
This is why we have so many different weight loss options, since medication is based on substances affecting different pathways, signals and weight management systems. One such drug, aimed at improving adipose tissue function and fatty acid metabolism is AOD9604.
AOD9604 is a modified form of human growth hormone fragment 176-191, developed to stimulate prolipid mobilizing and lipid oxidation (during which fatty acids decompose into carbonyl compounds, unsaturated aldehydes, ketones and other substances).
Even though AOD9604 has not yet been deemed FDA-approved,a number of studies showed its administration led to a significant weight loss and improvements in glucose tolerance (in both animal and early stage human studies).
Another such study done on 300 obese individuals in Australia showed that AOD9064 administration more than tripled weight loss in test subjects, compared to those on a placebo drug. Furthermore, this study proved that long-term treatment is not likely to cause resistance to AOD9064 based medication, making it a perfect candidate for future weight loss medication and treatment.
So far, animal and human studies both showed AOD9064’s effectiveness in helping test subjects lose weight, improve glucose tolerance, while presenting with minimal side effects. Further research studies are needed before including it into an FDA-approved treatment procedure, but the initial findings show a great potential.
Reference:
Michael D. Jensen. Potential Role of New Therapies in Modifying Cardiovascular Risk in Overweight Patients with Metabolic Risk Factors. 06 September 2012
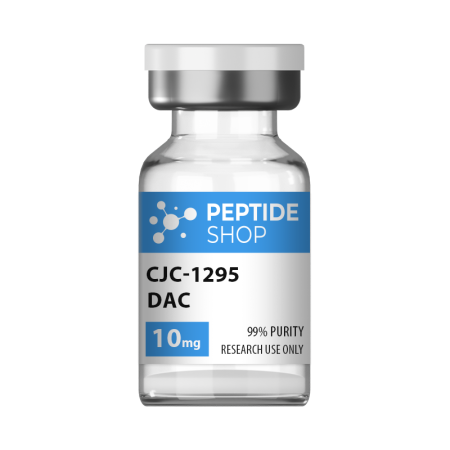
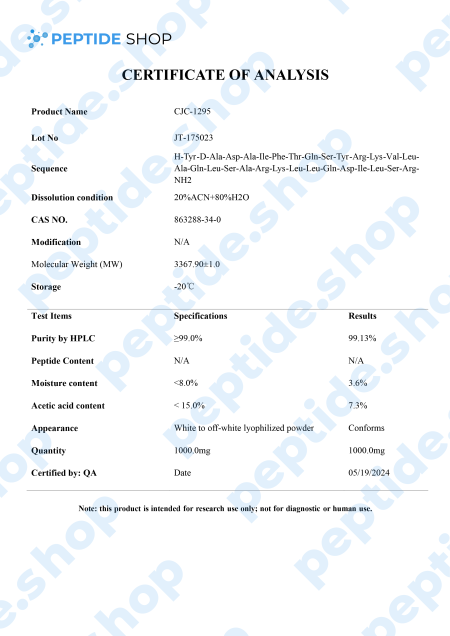
If you’re a peptide researcher (or plan on becoming one), you should know the difference between CJC-1295 and CJC-1295 DAC. CJC-1295 DAC features an additional component at the end of the peptide chain, also known as a drug affinity complex or DAC.
This small fragment changes the peptide’s functionality and extends its half-life to six to eight days. It might have a prolonged effect of up to two weeks.
Below, we will showcase the main similarities and differences between these two peptides, including their properties, characteristics, and mechanism of action.
What is CJC-1295 DAC peptide?
This peptide resembles the regular CJC-1925 since it is a modified form of natural GHGR (1-29). However, this one differs from CJC-1925. It has an additional molecule known as a “drug affinity complex.”
DAC features a couple of oxygen and nitrogen atoms connected by chemical bonds. According to some findings, this small number of atoms could significantly impact peptide breakdown rate and its use in the body.
What is CJC-1295 Peptide?
This peptide is also known as “modified growth hormone releasing factor (1-29)”, “ModGRF 1-29”, or “Modified GRF (1-29).” You may also encounter the name “CJC-1295, without DAC.”
All these names imply a specific peptide molecule containing a short amino acid chain. As many studies have indicated, this peptide may boost growth hormones in the bloodstream.
Growth hormone may have a significant role in several vital internal activities. It could facilitate cellular reproduction, repair, and growth, help with tissue repair, improve muscle cell development, support skin cells, and other functions.
While the body naturally produces growth hormone, this production tends to naturally decrease. According to some research done in laboratory settings, CJC-1295 may encourage the natural production of growth hormone, increasing its levels, which could lead to quicker repair, fat cell burn, and muscle cell growth.
Differences between CJC-1295 DAC and CJC-1295
As research studies have outlined, here are some fundamental differences between these two peptides.
Half-life
The main distinction lies in their half-lives. CJC-1295 is thought to mimic the body’s natural peptide. The endogenous GHRH has a short half-life of just a couple of minutes. Similarly, CJC-1295 has a brief half-life of around half an hour.
Regarding the second peptide, the additional DAC could significantly alter the organism’s peptide use. Researchers believe that DAC offers a peptide, a lysine linker, which could protect and prevent it from degrading.
Moreover, the DAC component could extend the half-life of this peptide to about six to eight days.
Properties of CJC-1295 DAC peptide
It is believed that CJC-1295 DAC boosts growth hormone levels in the bloodstream. Additionally, several studies suggest the following:
- Scientists and researchers need to focus their attention to studying the potential of growth hormones on growth and muscle recovery.
- Growth hormone may help convert fatty tissue into energy.
- Growth hormones are linked with collagen production in the skin, which means this peptide may also help with skin regeneration and skin cell development.
- CJC-1295 DAC may positively impact sleep patterns.
- Growth hormone is essential for tissue regeneration and helps the organism recover from damage.
References:
Teichman SL, Neale A, Lawrence B, Gagnon C, Castaigne JP, Frohman LA. Prolonged stimulation of growth hormone (GH) and insulin-like growth factor I secretion by CJC-1295, a long-acting analog of GH-releasing hormone, in healthy adults. J Clin Endocrinol Metab. 2006 Mar;91(3):799-805. doi: 10.1210/jc.2005-1536. Epub 2005 Dec 13. PMID: 16352683.
Sam L. Teichman, Ann Neale, Betty Lawrence, Catherine Gagnon, Jean-Paul Castaigne, Lawrence A. Frohman, Prolonged Stimulation of Growth Hormone (GH) and Insulin-Like Growth Factor I Secretion by CJC-1295, a Long-Acting Analog of GH-Releasing Hormone, in Healthy Adults, The Journal of Clinical Endocrinology & Metabolism, Volume 91, Issue 3, 1 March 2006, Pages 799–805,
American Journal of Physiology-Endocrinology and Metabolism 2006 291:6, E1290-E1294
Oxytocin, also known as the love hormone, helps us bond with our loved ones and is often released through touch, exercise, and music.
What is Oxytocin?
This natural hormone manages crucial aspects of male and female reproductive systems, including lactation, labor, delivery, and certain aspects of human behavior. The hypothalamus produces oxytocin, but the posterior pituitary gland releases and stores this hormone into the bloodstream.
Hormones are chemicals that manage various functions in the human body by carrying messages through blood to tissues, muscles, and organs. These signals instruct your body what to do and when to do it.
The hypothalamus is part of the brain that controls functions such as heart rate, digestion, body temperature, and blood pressure. On the other hand, the pituitary gland is a small, pea-sized endocrine gland placed at the base of the brain, below the hypothalamus.
Synthetic Forms of Oxytocin
A synthetic form of oxytocin is used in hospital settings, particularly when doctors need to induce labor in childbirth if it hasn’t begun naturally or to help with contractions. Healthcare providers may also use this hormone to speed up the delivery of the placenta, which is the third stage of labor, and minimize the risk of heavy bleeding.
Function of Oxytocin
As previously mentioned, the two main functions of oxytocin are to encourage uterine contractions in childbirth and labor and to boost contractions of breast tissue to help with lactation after childbirth.
However, apart from these, oxytocin has other important roles, such as:
- Placenta-infant bonding
- Romantic attachment
- Trust
- Recognition
- Sexual arousal
The effects of oxytocin on the human brain are complex, and scientists are currently researching the role of oxytocin in various conditions.
- PTSD
- Depression
- Autism spectrum disorder
- Anxiety
- Anorexia
- Addiction
Florea T, Palimariciuc M, Cristofor AC, Dobrin I, Chiriță R, Bîrsan M, Dobrin RP, Pădurariu M. Oxytocin: Narrative Expert Review of Current Perspectives on the Relationship with Other Neurotransmitters and the Impact on the Main Psychiatric Disorders. Medicina (Kaunas). 2022 Jul 11;58(7):923. doi: 10.3390/medicina58070923. PMID: 35888641; PMCID: PMC9318841.
Kendrick KM, Guastella AJ, Becker B. Overview of Human Oxytocin Research. Curr Top Behav Neurosci. 2018;35:321-348. doi: 10.1007/7854_2017_19. PMID: 28864976.
https://www.sciencedirect.com/science/article/pii/S0306453013002369
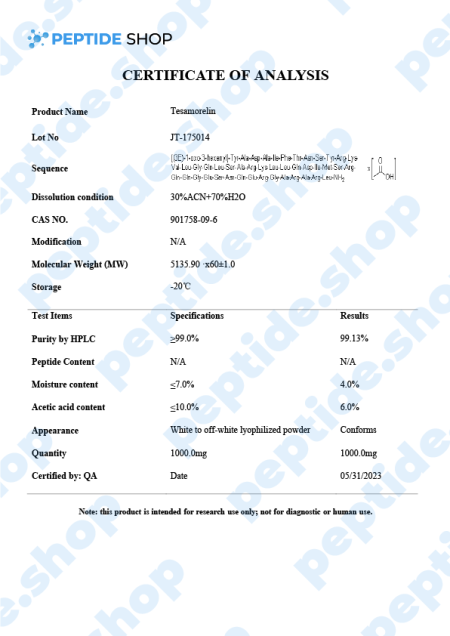
Tesamorelin is a 44 amino acid long, synthetic growth hormone releasing hormone (GHRH) analogue. It was primarily developed and used to treat visceral fat buildup in HIV positive patients suffering from lipodystrophy (a condition characterized by abnormal fat distribution).
Tesamorelin peptide activates GHRH receptors in the pituitary gland, resulting in growth hormone synthesis and release. This GH release further stimulates the production of Ilike growth factor-1 (IGF-1), which is naturally low in obese and diabetic patients.
The good thing about tesamorelin is that it was approved in the US back in 2010 for the treatment of abdominal fat in HIV positive patients as a part of the antiviral therapy-related lipodystrophy. It has also been evaluated as a potential therapy of insulin resistance, nonalcoholic fatty liver and, of course, obesity. These clinical studies are still ongoing and we’ll need more information to confirm its effectiveness.
The usual tesamorelin dosage for patients is 2mg given in the form of a subcutaneous injection, once a week. As for the side effects, patients did not report that many, but from the ones we have documented, most common are:
- Application site irritation
- Itching
- Peripheral edema
- Mild nausea
- Redness
More importantly, tirzepatide therapy was not associated with hepatotoxicity and is very unlikely to cause any clinically apparent liver injuries.
Reference:
Cagrisema 10mg is one of the latest PeptideShop’s peptide blends, which combines cagrilintide and semaglutide. Each vial contains a combination of lyophilized cagrilintide and semaglutide, 5mg each, tested for purity and strength, and suitable for lab experiments and chemical trials.
Semaglutide is a GLP-1 receptor agonist. GLP-1 is one of the main gut peptide hormones in humans, which plays a role in many different mechanisms within the body from insulin secretion, glucagon release, gastric emptying, appetite and energy intake.
And cagrilintdide is an amylin analogue co-secreted with insulin, which plays a role in glycemic control and gastric emptying.
Researchers hypothesize that this combination profoundly influences receptor changes in the brain, insulin secretion, appetite regulation and glucagon secretion.
Though this combination has not yet been fully tested, we have data from a study on the effects of Cagrisema on patients with type 2 diabetes.This was a 32-week, double-blind study across 17 sites in the USA, conducted on 92 individuals in total.
Final results showed that cagrisema resulted in clinically relevant improvements in glycaemic control (significant change in HbA1c) and, more importantly, a greater weight loss versus semaglutide as well as cagrilintide.
References:
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(23)01163-7/abstract
CJC-1295 is a synthetic analogue of growth hormone-releasing hormone (GHRH) and growth hormone secretagogue (GHS) developed by ConjuChem Biotechnologies.
GHRH is a 44-amino acid long peptide which our hypothalamus synthesizes and in the pituitary gland, it binds to the growth hormone (GH) receptors, resulting in the release, regulation and pulsatile secretion of GH.
We already talked about GH therapy as being FDA approved in conditions such as GH deficiency, Turner syndrome, Prader-Willi syndrome, idiopathic short stature etc. Recombinant human GH treatment is generally performed as one daily, subcutaneous injection which elevates the levels of GH serum in the blood.
One of the major problems with this approach to treatment is that the efficacy of GH therapy is hard to determine due to the lack of biological serum biomarkers. Currently, most facilities are using levels of IGF-1 and IGFBP-3 to monitor the efficacy of this therapy but these levels may vary wildly (due to growth velocity, glucose tolerance, insulin levels etc.).
Furthermore, GH abuse extended across multiple sports disciplines, making it even harder to suppress and put this problem under control.
Researchers hope to solve this problem by employing new biomarkers of GH action and secretion. One such way is to employ newly developed molecules, such as CJC-1295, shown to increase both GH and IGF-1 levels in the blood, without affecting the pulsatility of GH secretion. CJC-1295 also has a prolonged half-life of 8 to 10 days, due to its ability to bind to the endogenous serum albumin.
So, what scientists are hoping to achieve with CJC-1295 is both a safe way of promoting GH secretion as well as making it measurable in a laboratory setting. There were numerous studies tackling this issue, but we still need further testing to confirm these preliminary findings.
Reference:
Sackmann-Sala L, Ding J, Frohman LA, Kopchick JJ. Activation of the GH/IGF-1 axis by CJC-1295, a long-acting GHRH analog, results in serum protein profile changes in normal adult subjects. Growth Horm IGF Res. 2009 Dec;19(6):471-7. doi: 10.1016/j.ghir.2009.03.001. Epub 2009 Apr 21. PMID: 19386527; PMCID: PMC2787983.
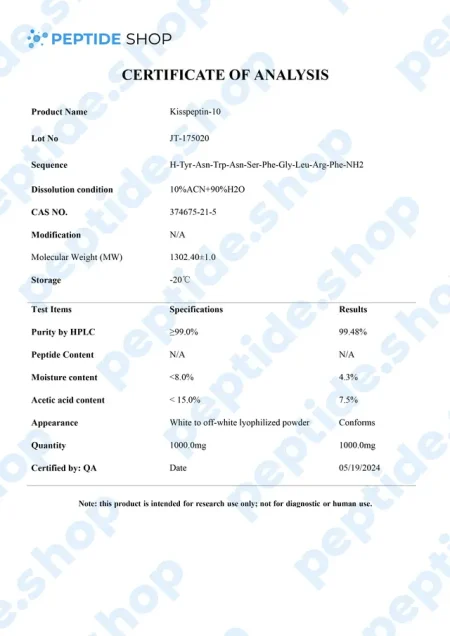
Metastin or Kisspeptin is believed to have the ability to prevent the spread of cancer or metastasis. This peptide is produced by the hypothalamus, which stimulates the release of GnRH or gonadotropin-releasing hormone, which then causes follicle-stimulating hormone and luteinizing hormone to be released from the purity gland.
Kisspeptin is used in testosterone replacement therapy instead of hCG to increase testosterone levels. That’s why it has emerged as a crucial regulator of the mammalian reproductive axis.
This peptide was first discovered in 1996 when it managed to inhibit melanoma cell lines. It belongs to a family of peptides that are derived from the KISS1/kiss1 gene structure, forming from prepro-kisspeptin, which has differential proteolysis for a common precursor.
Kisspeptin is classified as an RF or neuroactive peptide with a specific Arg-Phe-NH2 motif.
Benefits:
Kisspeptin binds to receptors in the pituitary gland, triggering a response that prompts the gland to release neurotransmitters, signaling the release of LH and FSH.
Based on numerous animal studies, scientists have managed to uncover the following benefits:
- Boosts the production of testosterone naturally
- Regulates fertility
- Increases sexual drive
- Improves immune response
- Boosts brain function
- Promotes weight loss
How does Kisspeptin work?
This peptide stimulates the release of GnRH or gonadotropin-releasing hormone. It enters the purity gland through receptor sites, causing a gland to release neurotransmitters, which later signal the releases of FH and LH. These hormones play a crucial role in the production of oestradiol and testosterone.
Kisspeptin mimics the action of hCG and clomiphene, and according to some animal studies, it can affect fertility in female and male animals.
Distribution of Kisspeptin
Kisspeptin was first found in the placenta, and later, it has been observed in the small intestine, pancreas, ovaries, and testis in mammals. The primary expression of Kisspeptin and its receptors have been shown in two big neuronal populations within the hypothalamus of rodents, the anteroventral periventricular nucleus and the arcuate nucleus.
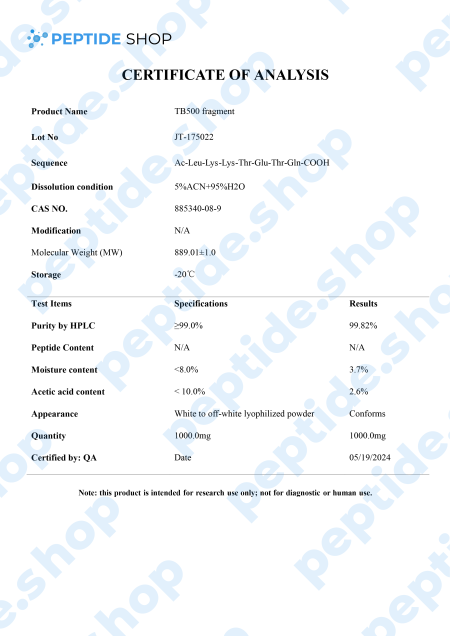
TB-500 is a 43 amino acid long synthetic peptide, analogue of thymosin beta-4. Thymosin beta-4 is a widely distributed peptide, and present in virtually all mammalian cells, which plays a pivotal role in many different processes in the body – it increases angiogenesis (formation of new blood vessels), proliferation, inhibits apoptosis (cell death) and inflammation.
Numerous animal clinical trials also showed that thymosin beta-4 can be used to indicate myocardial, liver and renal problems.
Angiogenesis:
Thymosin beta-4 promotes angiogenesis, triggers cell proliferation and migration, as well as the formation of capillary-like structures in cells. It also triggers blood perfusion (local fluid flow) by increasing capillary density.
Apoptosis:
Thymosin beta-4 inhibits apoptosis by inhibiting the transforming growth factor pathway. It also prevents nucleus pulposus (spinal disk providing shock absorption during movement) cell apoptosis and slows down cellular aging.
Inflammation:
In mouse models Tβ4 significantly dropped the number of inflammatory cells in the brains of the treated animals. It also prevented the production of proinflammatory cytokines and effectively blocked the increase of ethanol-induced inflammatory factors.
Heart Health:
Clinical data showed that thymosin beta-4 has a positive effect on both acute phase (immediately following the injury) where it preserves the ischemic myocardium, as well as in the chronic phase, in which it activates the growth of vascular cells.
After observing Tβ4’s benefits in animal models, it’s not surprising TB-500 gained so much popularity recently, since it acts as Tβ4’s synthetic analogue. Numerous clinical studies (in animal models) showed TB-500 as a potent way to improve blood vessel growth and fluid flow, accelerate wound healing, reduce oxidative stress and bind protein.
Of course, more research is needed to determine the full effects of this peptide, its safety and effectiveness in human test subjects.
Reference:
Xing Y, Ye Y, Zuo H, Li Y. Progress on the Function and Application of Thymosin β4. Front Endocrinol (Lausanne). 2021 Dec 21;12:767785. doi: 10.3389/fendo.2021.767785. PMID: 34992578; PMCID: PMC8724243.
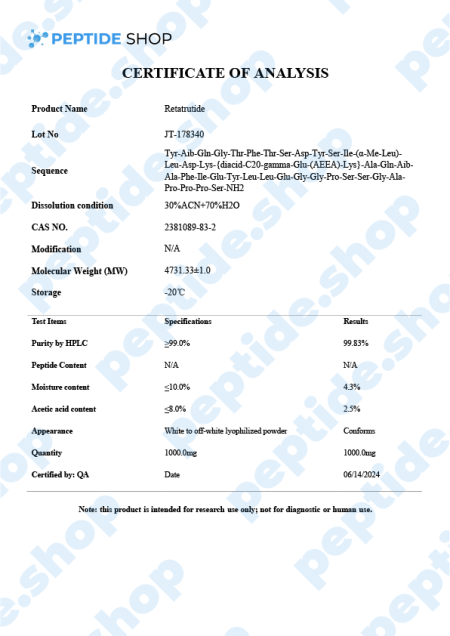
Retatrutide is one of the latest incretin mimetic drugs being tested for their weight reduction properties. Researchers use incretin mimetic agents as they work to mimic incretin hormones (gut peptides that get secreted after we eat) to allow for a better insulin secretion and hyperglycaemic control.
Even though there are numerous weight reduction agents being prescribed and used, FDA-recognized “treatment” for nonsyndromic obesity are:
- Orlistat
- Phentermine-topiramate
- Naltrexone‐bupropion
- Liraglutide and
- Semaglutide
With the exception of glucagon-like peptide 1 receptor agonists (such as semaglutide), most weight reduction agents come with a specific set of side effects such as nausea, gastrointestinal distress, abdominal pain, vomiting, diarrhea, or a general weight decrease that does not cross the 15% mark. Some of these medications even come with a warning against using them if a patient is suffering from a kidney, heart, thyroid or any related problems.
This is why scientists are turning more and more to retatrutide, because this incretin mimetic decreases appetite, promotes the feeling of fullness and slows down the process of gastric emptying, but does all that while presenting with minimal side effects and increased weight loss effectiveness, compared to liraglutide or semaglutide.
Retatrutide Mechanism of Action
Retatrutide exerts a powerful glucagon-receptor agonistic effect. When we compare it to human glucagon and glucagon-like peptide 1 (GLP-1), it exhibits:
- Reduced potency on the GCGR (human glucagon receptor) and GLP-1R (glucagon-like peptide-1 receptor)
- Enhanced potency at the human GIPR (gastric inhibitory polypeptide receptor)
When talking about in vitro experiments, retatrutide demonstrated similar efficacy in evoking glucose production within hepatocytes and inducing lipolysis. Also, retatrutide showed a favorable half-life of 6 days, enabling it a weekly dosage regimen (should the drug get FDA approved).
Another double-blind study conducted in the US on obese patients showed promising results. 338 adults in total were involved, split into 6 cohorts (depending on the weekly dosage), up against a placebo group. Retatritude group experienced the following results:
- 1mg group – after 24 weeks this group experienced weight loss of 7.2%, and after 48 weeks a total loss of 8.7%
- 4mg group (commencing with 2mg) – after 24 weeks this group experienced a weight loss of 11.8%, and after 48 weeks a total loss of 16.3%
- 4mg group (commencing with 4mg) – after 24 weeks this group experienced a weight loss of 13.9%, and after 48 weeks a total loss of 17.8%
- 8mg group (commencing with 2mg) – after 24 weeks this group experienced a weight loss of 16.7%, and after 48 weeks a total loss of 21.7%
- 8mg group (commencing with 4mg) – after 24 weeks this group experienced a weight loss of 17.9%, and after 48 weeks a total loss of 23.9%
- 12mg group (commencing with 2mg) – after 24 weeks this group experienced a weight loss of 17.5%, and after 48 weeks a total loss of 24.2%
In contrast, the placebo group only experienced a 1.6% weight loss after 24 weeks and 2.1% after 48. Findings also showed that adverse effects related to retratitude treatment (such as nausea, vomiting, diarrhea and constipation), were mild and depended on the dosage.
In conclusion, this peptide showed promising results in addressing obesity in both in vitro and human test subject studies. However, test samples were relatively small, and we still need more research and clinical trials to show the effectiveness of retratutide as an effective, long-term way of managing weight.
Reference:
Naeem M, Imran L, Banatwala UESS. Unleashing the power of retatrutide: A possible triumph over obesity and overweight: A correspondence. Health Sci Rep. 2024 Feb 5;7(2):e1864. doi: 10.1002/hsr2.1864. PMID: 38323122; PMCID: PMC10844714.
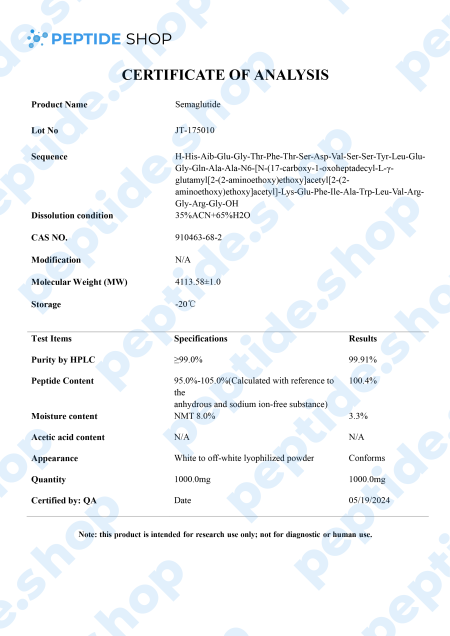
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist.It is one of the two primary hormones that may enhance incretin activity in rodent models, along with GIP.
GLP-1 is one of the major incretin (gut peptide secreted after nutrient intake) hormones in humans. It plays a pivotal role in many different mechanisms within the body:
- Insulin secretion
- Inhibits glucagon release (glucagon is secreted as a response in blood sugar drop)
- Suppresses hepatic gluconeogenesis (glycogen is the primary carbohydrate stored in the liver)
- Delays gastric emptying
- Reduces appetite and energy intake
When talking about obese diabetic 2 type patients, GLP-1 assumes a special status in their treatment as it lowers HbA1c levels along with body weight, but without the risk of hypoglycemia.
However, the biggest problem with GLP-1 is its short half-live (of only 1 to 2 minutes) and this is why researchers turner to various other GLP-1 receptor agonists, such as liraglutide, dulaglutide and, of course, semaglutide. Another thing researchers hope to achieve by turning to GLP-1 agonists, such as semaglutide, is to develop an effective diabetes management drug which needs less frequent dosing.
Murine models suggested that semaglutide’s GLP-1 receptor activation affects insulin secretion, blood sugar homeostasis and beta cell protection. Further, in vitro studies showed its potential to also affect glucagon secretion. This insulin glucagon mechanics is what’s used to balance our pancreatic function and regulate metabolism.
References:
- Mahapatra MK, Karuppasamy M, Sahoo BM. Semaglutide, a glucagon like peptide-1 receptor agonist with cardiovascular benefits for management of type 2 diabetes. Rev Endocr Metab Disord. 2022 Jun;23(3):521-539. doi: 10.1007/s11154-021-09699-1. Epub 2022 Jan 7. PMID: 34993760; PMCID: PMC8736331.
- Meier JJ. GLP-1 receptor agonists for individualized treatment of type 2 diabetes mellitus. Nat Rev Endocrinol. 2012 Dec;8(12):728-42. doi: 10.1038/nrendo.2012.140. Epub 2012 Sep 4. PMID: 22945360.
500 in stock


 Anti Aging
Anti Aging Hair Growth
Hair Growth Muscle Growth
Muscle Growth Peptide Blends
Peptide Blends Peptide Supplies
Peptide Supplies Peptides
Peptides Skin
Skin Testosterone
Testosterone Weight Loss
Weight Loss



Reviews
There are no reviews yet.